Table of Contents
Somnambulism, more commonly known as sleepwalking, is a parasomnia disorder characterized by performing physical actions such as walking while asleep. Sleepwalkers are often unaware of their actions and may have difficulty waking from their sleep. Although most episodes last only a few minutes, some can continue for 30 minutes or more.
Sleepwalking typically occurs during the first few hours of sleep, although it can also happen during naps. It is more common in children than adults, with the peak incidence between 3 and 8 years.
Somnambulism can also occur in adults, particularly during stress or fatigue. While the exact cause of somnambulism is unknown, it is believed to be associated with disruptions in the normal sleep cycle. Treatment is typically unnecessary unless the sleepwalker is at risk of injuring themselves or others. In such cases, measures such as bedtime sedatives or increased supervision may be recommended.
Safety is a big concern for sleepwalkers, and it may worthwhile to consider limiting their mobility by limiting access to doors and windows.
Is somnambulism a type of parasomnia or sleep disorder?
Parasomnia is a sleep disorder characterized by abnormal motor or verbal behavior during sleep. Somnambulism, or sleepwalking, is the most well-known form of parasomnia, but there are other types, including sleep terrors, sleep eating and teeth grinding. Parasomnias can occur in all age groups, but they are most common in children. Parasomnias often run in families, so there is likely a genetic component to the disorder.
What are the symptoms of sleepwalking?
The symptoms of sleepwalking can include the following:
- Walking around while asleep
- Sitting up in bed with eyes open but being unresponsive.
- Performing complex tasks such as cooking, driving or even fighting while asleep.
- Not remembering anything that happened while sleepwalking
- Having a blank expression on your face
- Being confused and disoriented after waking from a sleepwalking episode.
What can cause sleepwalking?
Several factors can contribute to somnambulism, including sleep deprivation, stress, sleep apnea, medication, and genetic predisposition. Sleepwalkers are more likely to have a family history of somnambulism.
What are the dangers of sleepwalking?
There are a few dangers of sleepwalking that you should be aware of.
- Sleepwalkers can hurt themselves or others while they are sleepwalking. For example, they may fall down the stairs or run into something in the dark.
- Sleepwalking can cause people to do things they wouldn’t normally do. For example, they may eat something they’re allergic to or go outside without a coat in cold weather.
- Sleepwalking can lead to exhaustion and sleep deprivation if it’s frequent enough. This is because it can disrupt a person’s normal sleep pattern and make it harder for them to get restful sleep.
- Sleepwalkers may disrupt another person’s sleep, especially if they are a concerned family member. The disruption may be purely physical, such as noise, but may be disruptive because of the worry and anxiety that a caretaker might have for the sleepwalker.
What are the causes of Sleepwalking?
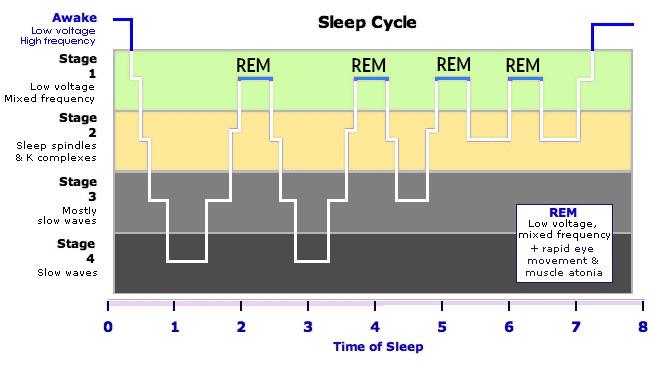
Sleepwalking generally happens in the deep stages of sleep (stage 3 and 4). Nobody knows exactly how someone begins to sleepwalk.
Contributing factors that cause sleepwalking include the following:
- Schedule changes or jetlag
- Stress
- Fever
- Sleep deprivation.
- Substance abuse, including alcohol.
- Genetics. Sleepwalking tends to run in families, especially if both parents of the afflicted person has experienced sleepwalking episodes in their lifetime.
Some conditions may trigger sleepwalking episodes. These conditions include:
- Obstructive sleep apnea. This is a breathing disorder that occurs during sleep.
- Use of medication that is used to treat psychiatric disorders.
- Restless leg syndrome.
- Gastroesophageal reflux disease.
Treatment and prevention for Sleepwalking
Improve sleeping habits to treat sleepwalking
Improving sleeping habits to eliminate sleepwalking is something anyone can do at no cost and with little effort. Some of the changes require some sacrifice, but that is in the eye of the beholder.
Quick and easy changes you can make today include:
- Have a consistent bedtime and a sleep schedule that allows for 7-9 hours of sleep. The hours of sleep you need to feel well-rested varies from person to person, but scheduling more time than you think is better than waking up tired from too little sleep.
- Avoid alcohol and caffeine at least 4 hours before bed.
- Turn off electronic screens at least an hour before bed. You can still listen to relaxing music or talk radio.
- Dim the lights and use bulbs that have a warm color temperature (usually more orange color).
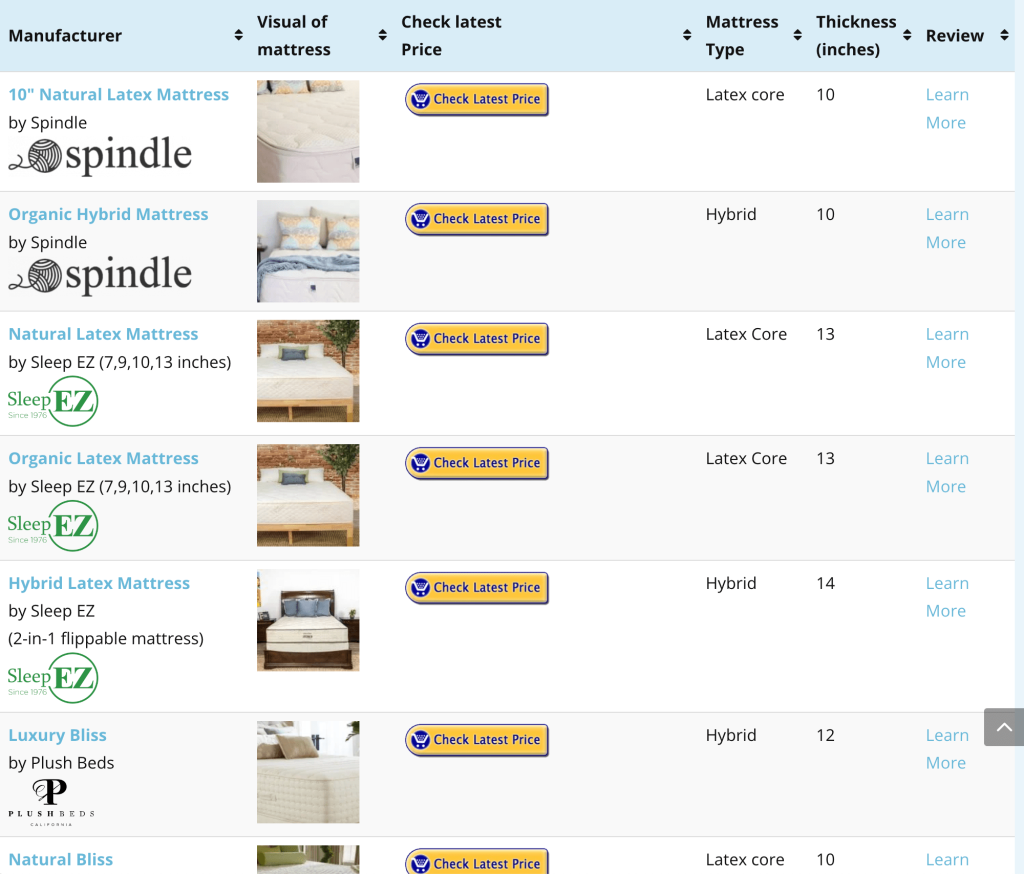
Improving the quality of your mattress is one of the ways to dramatically improve the quality of your sleep. A natural latex mattress will give you the most supportive, pressure-relieving feel. Additionally, natural latex mattresses are breathable, non-toxic, and more durable than polyurethane mattresses.
Cognitive Behavioral Therapy to treat sleepwalking
Cognitive behavioral therapy is a talking therapy that aims to reduce negative thoughts and behaviors related to depression and anxiety.
The CBT method for sleepwalking involves identifying negative thoughts about sleep and replacing them with positive thoughts. For example, the bed should be only used for sleep and nothing else. If the sleepwalker wakes up feeling distraught, relaxing, comforting thoughts and beliefs can be instilled and affirmed before returning to bed.
CBT is evidence-based and has been shown, in some cases, to be as effective, if not more effective, than medication.
Cognitive behavioral therapy may be effective in relieving stress and anxiety. CBT relaxation techniques may help eliminate sleepwalking episodes that are rooted in feelings of stress and anxiety.
Scheduled awakening for sleepwalking
Sleepwalking, sleep talking, sleep terrors and confusional arousals are all manifestations of the same sleep disorder called partial arousal parasomnias. The term means partially awake and, in the same light, partially asleep or midway between awake and asleep.
Sometimes, it is possible to communicate with and guide a child that is sleepwalking or having partial arousal parasomnia. If they are communicative, they may be confused or upset. The child may appear awake, but they are still sleeping through the events. Even though a child may be saying things that do not make sense, they are not dreaming.
Scheduled awakening is best used when a child has the same partial arousal parasomnias occurring around the same time. Scheduled awakening consists in
- monitoring the child’s sleep, wake, and episode time for 2 weeks.
- Designate the scheduled awakening time 15 -30 before the average parasomnia episode.
- Gently wake the child at the designated time.
- Once the child is awake (opening their eyes or telling you that he is awake), allow them to return to sleep.
Should I wake someone up that is sleepwalking?
Sleepwalking can be very dangerous, especially if there are stairs or sharp objects nearby. Sleepwalkers can trip over objects while moving around.
The best action to take is gently guiding the person back to bed. Someone that is sleepwalking may be difficult to wake up because they are in the deep, NREM phase of sleep. If it is absolutely necessary to wake the person up, it must be done gently, without startling them.
When do people start sleepwalking?
There are 4 stages of sleep:
- Stage 1 Non-rapid eye movement (NREM). You are transitioning from being awake to being asleep.
- Stage 2. NREM. In this stage, your heart rate slows, and your body temperature drops.
- Stage 3. NREM. This is the deepest stage of sleep. Your brain activity slows down, and your muscles relax.
- Stage 4. REM. Dreams occur in this final stage of sleep. Even with increased brain activity, your body is still immobilized. Eyes move around rapidly in this stage.
Sleepwalking occurs in Stage 3 and 4. NREM sleep.